Senior Sex Guide: Maintaining Sexuality and Intimacy After 60
Sexuality and intimacy are two subjects people rarely associate with older people. This stigma stems from the notion that as people age, they start losing interest in them. Thus, seniors who do show an interest in sex are called derogatory names and viewed as improper.
The truth is, age doesn’t matter when it comes to sexuality. While the ability to perform sexual activities may decline along with physical changes brought by aging, many seniors are still enthusiastic about sex.
In this article, readers will be able to dispel misconceptions about seniors and sexuality, learn about the normal sexuality changes as people age, how to deal with them, and how to regain one’s sexuality even after 60.
Let’s Talk Numbers: Sex and Aging Statistics Among Men and Women

Aging can cause normal physical changes that affect how people do sex, especially in their sexual organs. Senior men may find themselves having difficulty with getting and keeping an erection.
On the other hand, older women may notice narrowing and dryness in their vaginas. Menopause is also another factor that affects sexual desire.
According to HealthinAging.org, other factors that affect sex life in senior women include the following:
- Low sex drive among 50% of women aged 75–85 years
- Inability to climax among 4 out of 10 women
- Menopause-related sexual issues, such as a lack of interest and pleasure during sex
- Cultural influence that older women should not encourage sexuality
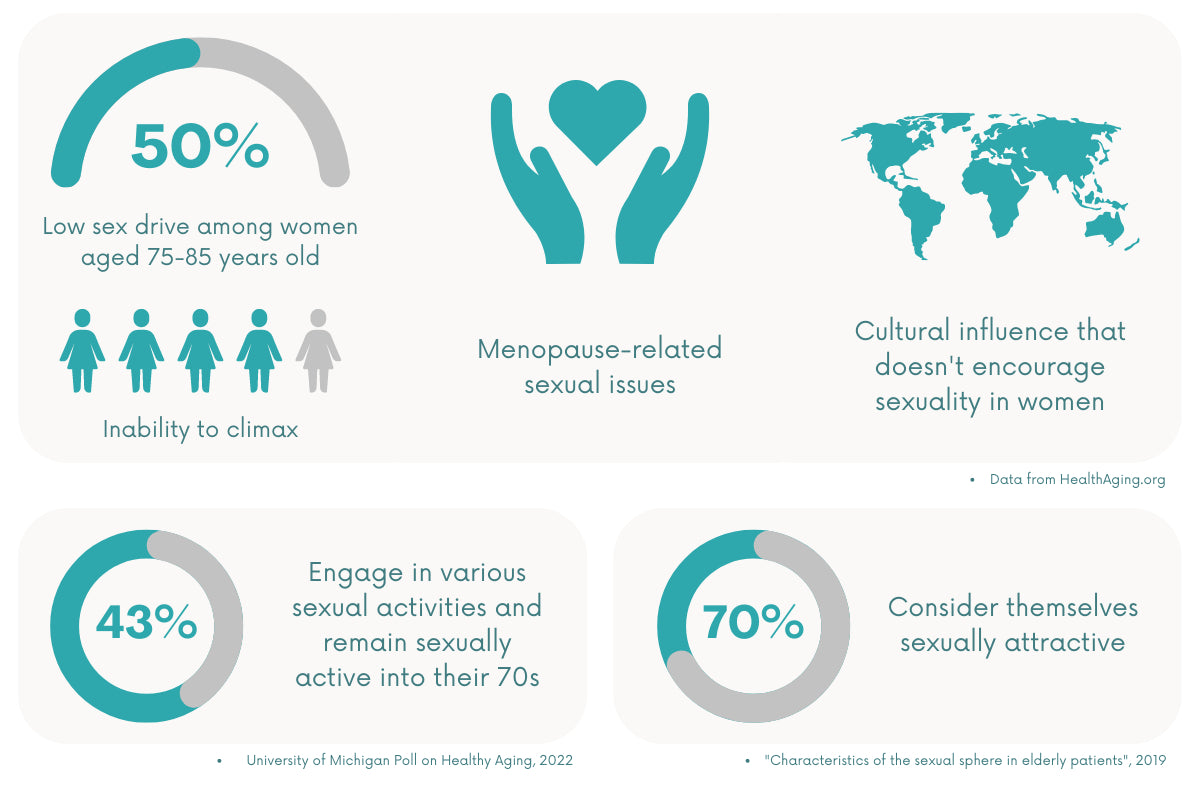
Despite these changes, it remains possible for seniors to show interest and engage in sexual activities. A recent report suggested that many women remain sexually active into their 70s. Around 43% still engage in sexual activities, whether intercourse, masturbation, or caressing. The rest of them are limited by age-related issues.
Another 2019 survey shows that sexual activity is essential for those over 60. In fact, 70% of the senior respondents consider themselves sexually attractive.
Correlation Between Aging and Sexuality
Seniors may experience newfound freedom to express themselves sexually after 50. For women, not having to worry about becoming pregnant is one reason. Chances are, seniors will have become more aware of what pleases them and their partners too.
But it’s no news how physical changes that come with aging greatly affect one’s sexual experience, especially among women. Below are some issues that occur in most people over 60.
How Does Sexuality Change with Age?
About half of the women ages 57 to 73 had sex less than twice a month several years prior to a 2021 Harvard Health report. Different factors can cause this decline in sexual drive, yet menopause seems to be one of the major culprits.
Menopause occurs in women usually between the ages of 45 to 55, but it can come earlier for some. Other women also experience this due to prior surgeries involving removal of the ovaries or uterus and undergoing cancer treatments.
Menopause marks a huge milestone in a woman’s life. But it also comes with uncomfortable changes that inhibit her sexuality.
Decline in libido
A few women have experienced increased libido after menopause without the worry of unwanted pregnancy and with most of their children already out of the home.
However, the majority notice having a lesser interest in sex than they did before this life change. With menopause, women experience a nosedive in estrogen levels and experience a variety of symptoms that significantly impact their sexual desire.
Discomfort during intercourse
The decrease in estrogen and progesterone levels—produced by the ovaries before menopause—also causes various symptoms that cause discomfort during sex. Vaginal dryness can cause intercourse to be a painful experience, which may lower the motivation to have sex while not necessarily the sexual drive.
Mood changes
Women reportedly experience twice as many bouts of depression as men. This usually occurs during major life changes, such as puberty, pregnancy and childbirth, and menopause.
There is still conflicting research around depression and its direct relation to menopause. However, hormone fluctuations and body image concerns are all possible causes of emotional distress among women undergoing menopause.
Benefits of Intimacy for Older Adults
While aging can cause barriers to sexuality, it does not diminish one’s intimacy with their partner. Being intimate with a loved one contributes to a happy and healthy relationship, whether through emotional (e.g., shared experiences) or physical means (e.g., cuddling, sexual intercourse).
In turn, it also provides several health benefits, especially for older adults:
- Less stress. Having ample social and emotional support from a partner strengthens one’s capacity to handle stress.
- Better healing. Whether to provide care or psychological support, having a committed partner promotes better healing in times of illness, treatment, or surgery.
- Lowers risk of depression. With consistent social support, seniors are less likely to experience emotional issues, such as anxiety and depression.
Sexual Health Concerns for Seniors

Like younger people, older adults can also experience their fair share of sexual health issues due to their age.
Physical Health Concerns
Vaginal dryness increases a menopausal woman’s chances of catching a sexually transmitted disease (STD), particularly AIDS caused by HIV. With less lubrication in the vagina, friction during sex can easily cause tearing and abrasions. Without proper hygiene, an infection may occur.
Since postmenopausal women do not worry about getting pregnant anymore, they’re less likely to use condoms during intercourse. This further exacerbates the risk of catching HIV and other STDs.
AIDS
Many senior adults think they are not as equally at risk for AIDS as the younger demographic. This may come from the notion that they have not been as sexually active. However, HIV does not choose its victim. People of any age can become infected by HIV, especially when they are sexually active.
Older people are more at risk of getting infected with HIV with their already weakening immune system. Getting the disease makes them even more susceptible to all kinds of health problems and serious diseases like cancer.
Other STDs
Seniors are not exempted from STDs, such as chlamydia, gonorrhea, syphilis, and hepatitis A and B. In fact, a 2020 report showed a historic high increase in STI rates among older Americans. This increase in STDs among seniors can cause an alarming array of health concerns, such as heart disease and cancer.
Emotional Health Concerns
Around 23 percent of women experience mood swings as they go through menopause, with irritability being their main emotional concern. This rollercoaster of emotions that happens to many senior women can affect how they view themselves sexually, as well as their attitudes toward sexual activities.
Aging can be a sensitive topic for many older adults, especially women undergoing menopause. While some handle this significant milestone with grace, others cannot take the end of their childbearing days lightly. Add to that the physical changes that lead to low self-esteem and confidence.
What Causes Sexual Problems in Seniors
Many factors lead to sexual issues among older adults. These can be categorized into four primary categories: illnesses, disabilities, medications, and surgeries.
Illness
Illnesses, like diabetes and heart disease, are some of the common causes of sexual problems. Diabetes can also cause sexual problems. When left uncontrolled, blood sugar levels can spike and cause a burning sensation and itching in the genital area. These symptoms can develop into a yeast infection that causes discomfort during sex.
Seniors with heart disease often experience erectile dysfunction (ED), as their illness causes a decrease in blood flow to the genital areas. Fear of a heart attack is also common among this demographic, which causes them to dispel the thought of having sex altogether.
Disabilities
Chronic illnesses, lifestyle, and other factors can lead to frailty among the elderly, which greatly impacts their sexual desire and performance. Disability can come from different types, including the following:
- Arthritis
- Foot problems
- Heart conditions
- Vision impairment
- Cognitive impairment
- Hearing impairment
- Hip fracture
- Chronic obstructive pulmonary disease (COPD)
For instance, arthritis can cause body stiffness, making sex uncomfortable or even painful for seniors. Chronic pain makes intercourse and foreplay more difficult as the body cannot function as it used to.
Medicine
Allergy medications, antidepressants, and hypertension (high blood pressure) treatments can affect sexual health. In addition, allergy drugs and sleep aids, appetite suppressants, cancer, and ulcer medications may negatively affect one’s sex life.
Suppose an older adult struggles with difficulty feeling aroused, has lost a desire for sex, or doesn’t feel any lubrication in their vaginal area. In that case, a healthcare professional can provide another possible solution.
Surgeries
Any invasive procedure can temporarily hamper a woman’s intimate life, especially surgeries like mastectomy and hysterectomy.
Mastectomy, which is often used to treat breast cancer patients, is the partial or total removal of the breast tissue, lymph nodes, areola, and nipple. On the other hand, hysterectomy has been linked to an increased risk of depression and anxiety.
Having a sexual or reproductive organ removed can contribute to disinterest or dissatisfaction with sex and intimacy, especially for seniors.
Possible Solutions for Sexual Problems
Although older adults experience different forms of sexual conditions, they shouldn’t be a hindrance to a healthy intimate life. There are solutions, whether their sexual problems stem from hormonal changes or other reasons.
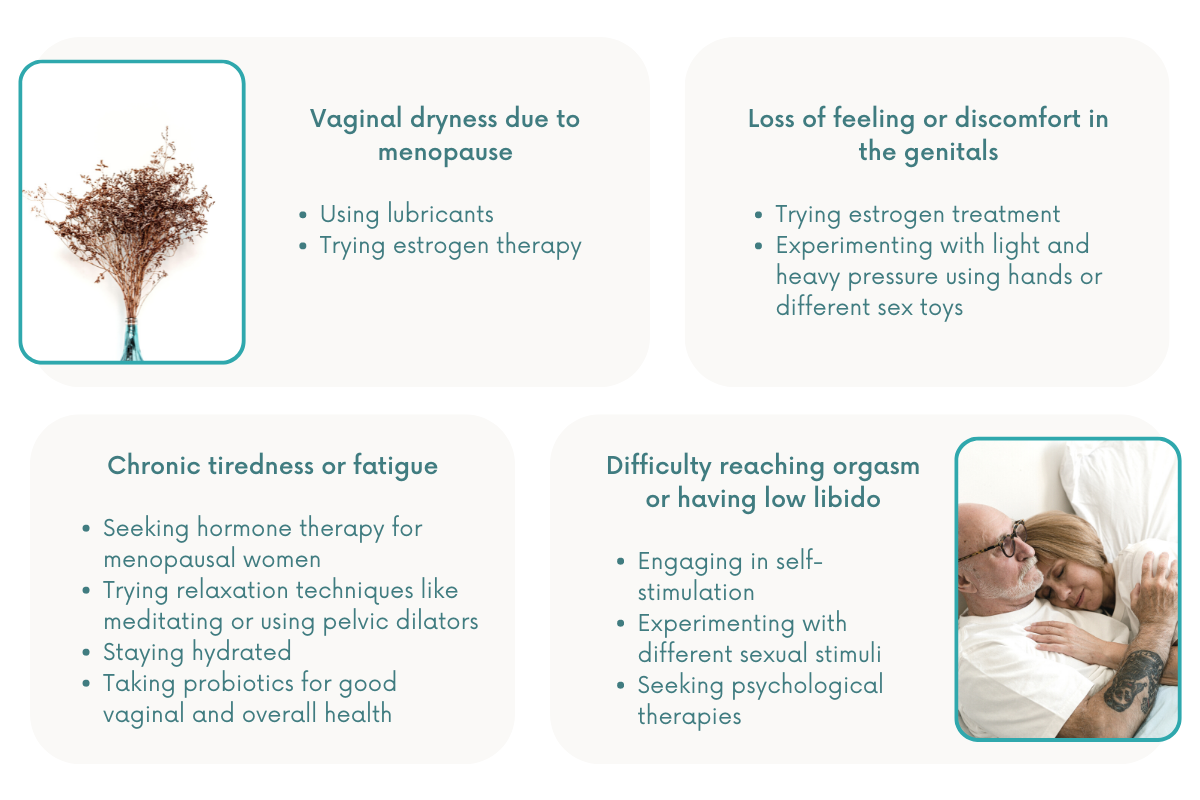
Vaginal dryness
As women age or go through menopause, hormone changes cause the vaginal walls to produce less lubrication resulting in vaginal dryness.
As this hampers their sexual life, older women can use lubricants to make sex more comfortable. Lubricants come in different types: water-based, silicone-based, and oil-based. Water-based lubricants are the safest option for intercourse and masturbation, while silicone-based ones are longer lasting.
Some women also try estrogen therapy via creams, pills, or an estrogen-releasing ring, to address dryness in the vagina.
A loss of feeling or discomfort in the genitals
For some women, estrogen treatment can alleviate vaginal burning and lessen pain during intercourse. Topical estrogen creams help heighten the senses in the clitoral region for senior women.
Another natural, unique approach is applying different degrees of touch to the body. Senior women can start exploring how their body responds to light and heavy pressure by using their hands or different sex toys. They can also let their partner participate in this activity to get constructive feedback.
Difficulty reaching orgasm or low libido
Seniors may experience reduced sexual desire, finding it more difficult to reach orgasm as they age. Such problems are usually treated with self-stimulation and psychological therapies.
Doctors may suggest experimenting with other sexual stimuli, such as role-playing, videos, pictures, vibrators, and fantasies. Older women may also be advised to learn more about their bodies and explore ways to arouse themselves. Stimulation of the clitoris is often all that is needed to achieve this.
Fatigue
Fatigue often stems from a poor diet and a sedentary lifestyle. Older men and women need to alleviate their exhaustion to boost their sexual desire and performance.
Chronic tiredness is difficult to overcome but not impossible. Aside from switching to a healthier lifestyle with proper diet and exercise, seniors can also try the following remedies:
- Hormone therapy for menopausal women
- Relaxation techniques like meditating or using pelvic dilators
- Staying hydrated
- Probiotics for good vaginal and overall health
Maintaining Sexual Health After 60
Maintaining a healthy sexual life can be challenging for seniors, but it may be easier to achieve with the right tips and medical interventions.

Tips for Improving One’s Sexual Life
Communicate with your partner
Healthy talks with their partners may help seniors solve their sexual issues. But this is often easier said than done. Feelings of self-consciousness and defensiveness may arise, which may result in avoidance. To achieve resolution, they may want to consult a third party, such as a counselor or therapist, to help with discussions about sex.
Seek professional help
One’s sexual problems may come from underlying physical conditions. Therefore, medical intervention should be considered. Seniors can talk to a doctor or a nutritionist about diets, medications, or exercises.
Some women even try the Kegel routines, which require clenching vaginal muscles to improve their function. To try this, practice while urinating and stop the urine from flowing through those muscles. Regular tests and general physicals are also important.
Regular Medical Tests for Older Women
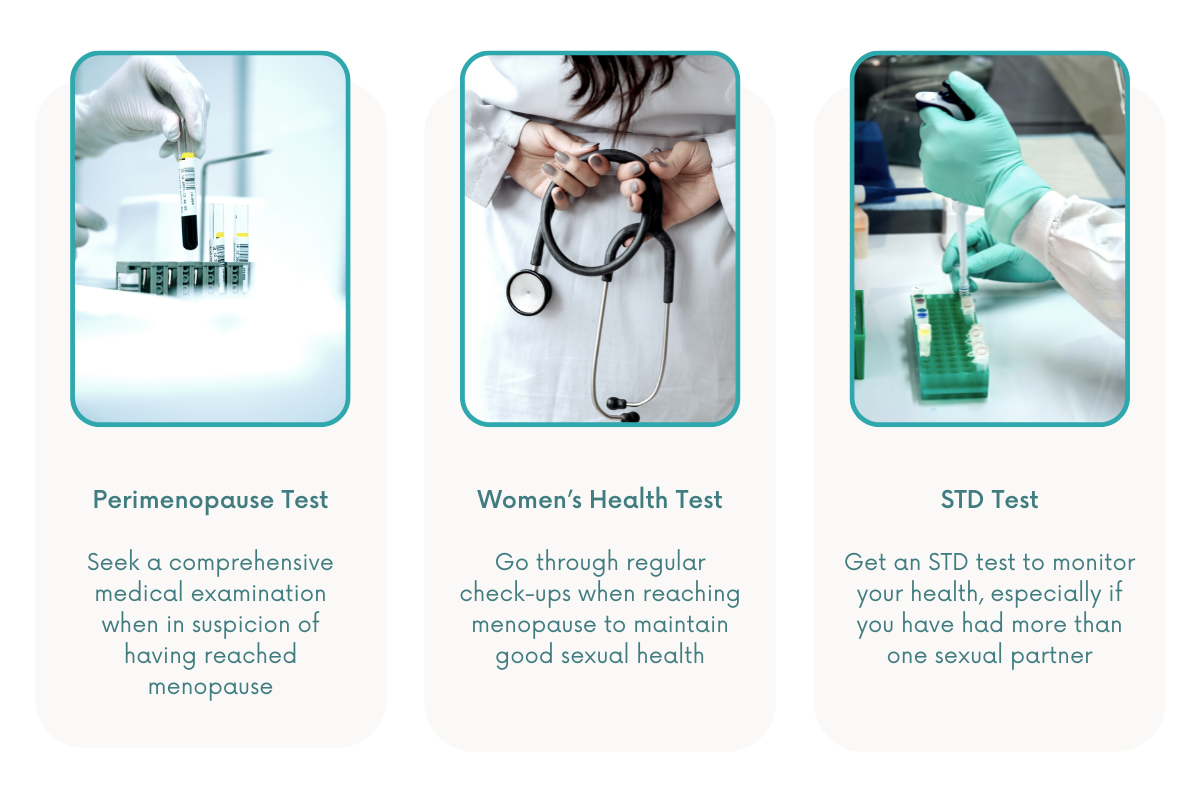
Perimenopause Test
There is no simple hormone test that diagnoses perimenopause for women. Hormone levels change throughout one’s menstrual cycle, making hormone tests unreliable.
Salivary hormone level tests may be considered, but they are inaccurate and should not be used to assess menopause symptoms.
Salivary hormone level tests may be considered, but they are inaccurate and should not be used to assess menopause symptoms.
The bottom line is that women shouinsa mld consider getting a comprehensive medical examination once they suspect they have already reached menopause.
Women’s Health Test
Regular well-woman checkups are essential in maintaining good sexual health, especially once a woman reaches menopause. During these examinations, a doctor will review their medical history, watch out for significant signs and symptoms, and prescribe appropriate treatment and medications.
STD Test
The Center for Disease Control says women ages 13–64 should test for HIV at least once. Individuals who have had sex with more than one partner may need to renew their test after six months with a new person.
The most common STD tests are for chlamydia, gonorrhea, and trichomonas. Testing for STDs often happens simultaneously when one receives a pap smear, which tests a woman for cervical cancer.
During an STD test, the cervix or vaginal wall is swabbed, but the sample may also be taken from the mouth or the rectum. During a well-woman exam, women are also advised to get a blood test to detect syphilis or hepatitis B and C, which are common STDs that may dampen a person’s sexual life.
Practicing Safe Sex for Seniors

Seniors may not think they are at risk when having sex. However, individuals can catch sexually transmitted infections (STIs) even if two people know each other and don’t have sex often.
Healthy Ways to Prevent STIs
STDs or STIs are acquired through sexual contact but may pass from person to person via blood, semen, and other bodily fluids.
An older adult with STI may or may not develop symptoms, which is why seniors must get themselves checked by a healthcare professional regularly. An STI that goes unnoticed and untreated may become more severe in the future.
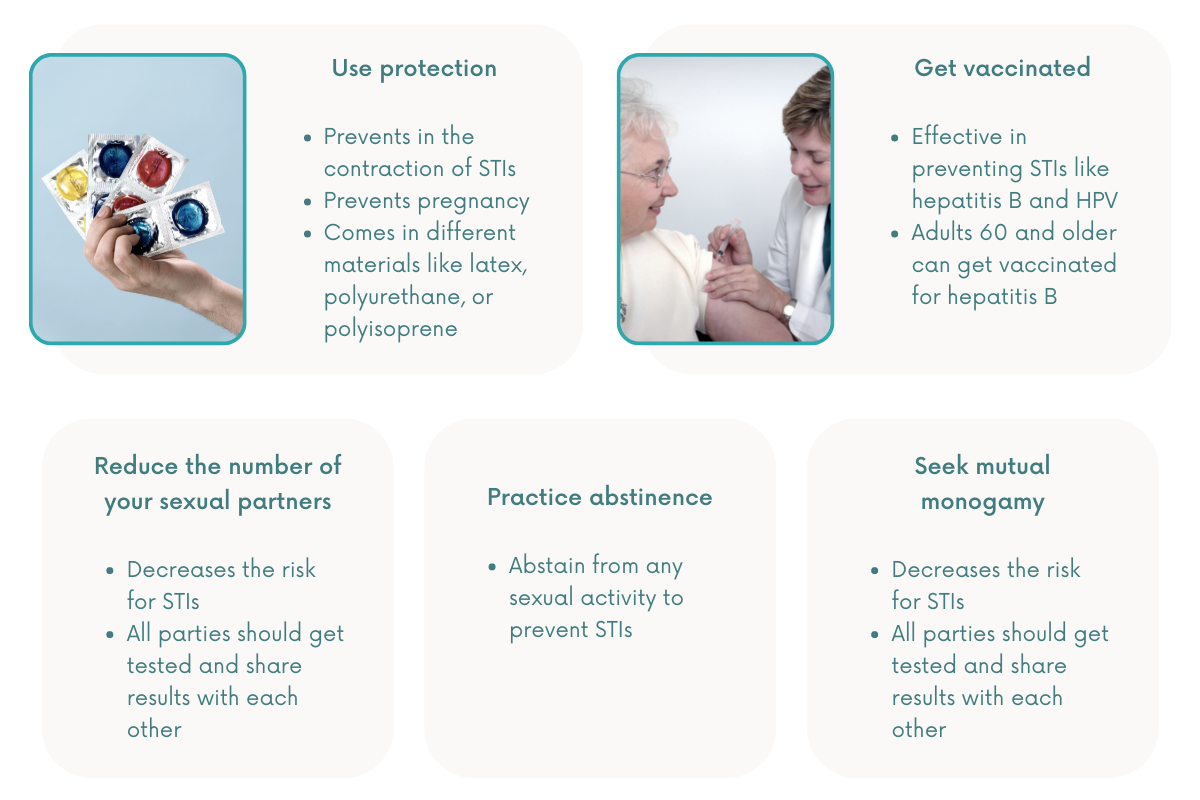
Aside from getting regular checkups, seniors must practice the following prevention tips:
Protection
Condoms are 98% effective in preventing pregnancy and STIs during sexual intercourse. External condoms, sometimes called male condoms, are made with very thin latex designed to keep semen from coming into contact with one’s sexual partner.
Those who are allergic to latex can try using a plastic condom made with polyurethane or polyisoprene. Beware of lambskin condoms, though, as they are too porous and are not as effective at safeguarding a person from STIs.
Vaccination
Vaccines are effective in preventing STIs like hepatitis B and HPV. However, HPV vaccination is only recommended for people ages 11 or 12 through 26. Some doctors may recommend it to adults ages 27 through 45, but only if they are at risk for new HPV infections.
On the other hand, older adults aged 60 and older can also get vaccinated for hepatitis B, especially if they have risk factors for such infection.
Reducing the number of sexual partners
Having multiple sex partners increases one’s risk for STIs. Aside from reducing the number of partners, it’s recommended for all parties to get tested and share their results with each other.
Mutual monogamy
Being sexually active with only one person helps decrease one’s risk for STIs. However, it’s also important for their partner to agree to this mutual monogamy. The most reliable way to prevent an infection is to be in a long-term monogamous relationship with an uninfected partner.
Abstinence
The most effective way to prevent an STI is to not have sex—be it anal, oral, or vaginal.
Recognize When You Need More Help
Aging can seem scary for women, especially as they undergo major physical and psychological changes. For those who feel apprehensive about their sexual health or their intimate life, it’s always best to seek professional help.
Helplines
- American College of Obstetricians and Gynecologists (Hotline: 800-673-8444)
- Senior Connection Center Inc. Elder Helpline (Hotline: 1-800-96-ELDER)
- National Institute on Aging (Hotline: 800-438-4380)
- Office on Women’s Health (Hotline: 202-690-7650)
- The North American Menopause Society (Hotline: 440/442-7550)
- Center for Disease Control and Prevention (Hotline: 800-CDC-INFO)
- Eldercare Locator (Hotline: 1-800-677-1116)
Helpful Resources
- Same-Sex Partnerships and the Health of Older Adults
- Sexual Health Care for Older LGBTQIA+ Adults
- Sexuality in Older Adults
- Sex Life Tips for People with Disability
- How to Discuss Sex with Elderly Patients
- A Guide for Aging Services Providers
- Programs and Services for Older Adults
- The Aging in Place: Growing Older at Home
References
- ACRIA. (2017, January). Older Adults and Sexual Health: A Guide for Aging Services Providers. https://www.health.ny.gov/diseases/aids/general/publications/docs/sexual_health_older_adults.pdf
- American Geriatrics Society. (2020, September). Basic Facts about Sexual Health | Aging & Health A-Z. HealthinAging.Org. https://www.healthinaging.org/a-z-topic/sexual-health/basic-facts
- CDC. (2021, December 14). Which STD Tests Should I Get? https://www.cdc.gov/std/prevention/screeningreccs.htm
- Conn, A., & Hodges, K. R. (2022, July 1). Orgasmic Disorder in Women. MSD Manual Consumer Version. https://www.msdmanuals.com/home/women-s-health-issues/sexual-dysfunction-in-women/orgasmic-disorder-in-women
- Estes, C. (2020, February 25). Historic High Rates Of STI’s Among Older Americans. Forbes. https://www.forbes.com/sites/claryestes/2020/02/26/historic-high-rates-of-stis-among-older-americans/?sh=556c8f504c39
- FamilyDoctor.Org Editorial Staff. (2022, April 22). Sexuality in Older Adults. FamilyDoctor.Org. https://familydoctor.org/sexuality-in-older-adults/
- Furst, J. (2019, September 5). Study Finds Women at Greater Risk of Depression, Anxiety after Hysterectomy. Mayo Clinic News Network. https://newsnetwork.mayoclinic.org/discussion/study-finds-women-at-greater-risk-of-depression-anxiety-after-hysterectomy/
- Harvard Health. (2021, September 30). Yes, You Can Have Better Sex in Midlife and in the Years Beyond. https://www.health.harvard.edu/womens-health/yes-you-can-have-better-sex-in-midlife-and-in-the-years-beyond#:%7E:text=Several%20years%20ago%2C%20a%20large,twice%20a%20month%2C%20on%20average
- Hernández Carrasco, M., de la Fuente Ballesteros, S., García Granja, N., Hidalgo Benito, A., García Álvarez, I., & Cano Pazos, M. (2019). Características de la esfera sexual en pacientes adultos mayores. Medicina de Familia. SEMERGEN, 45(1), 37–43. https://doi.org/10.1016/j.semerg.2018.09.007
- Johnson, T. (2002, October 7). Hormone Replacement Therapy for Menopause. WebMD. https://www.webmd.com/menopause/guide/menopause-hormone-therapy
- Kim, P. (2021, November 9). STD Testing. Testing.Com. https://www.testing.com/std-testing/
- Markopoulos, C., Tsaroucha, A., Kouskos, E., Mantas, D., Antonopoulou, Z., & Karvelis, S. (2009). Impact of Breast Cancer Surgery on the Self-Esteem and Sexual Life of Female Patients. Journal of International Medical Research, 37(1), 182–188. https://doi.org/10.1177/147323000903700122
- Mayo Clinic Staff. (2019, January 29). Depression in Women: Understanding the Gender Gap. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/depression/in-depth/depression/art-20047725
- Morales-Brown, L. (2020, August 13). The Best and Worst Lube Alternatives. Medical News Today. https://www.medicalnewstoday.com/articles/what-can-i-use-instead-of-lube
- Mudge, L. (2022, April 6). Probiotics for Women: What Are the Benefits? Livescience.Com. https://www.livescience.com/probiotics-for-women
- National Council on Aging. (2021, December 15). Intimacy and Older People. https://www.ncoa.org/article/why-is-intimacy-important-in-older-adults
- National Institute on Aging. (n.d.). Sexuality and Intimacy in Older Adults. https://www.nia.nih.gov/health/sexuality-and-intimacy-older-adults
- National Institute on Aging. (2021, September 1). HIV, AIDS, and Older Adults. https://www.nia.nih.gov/health/hiv-aids-and-older-adults#what
- NHS website. (2022, March 29). Condoms. NHS.UK. https://www.nhs.uk/conditions/contraception/male-condoms/
- North American Menopause Society. (n.d.). Depression, Mood Swings, Anxiety, Sexual Side Effects of Menopause. https://www.menopause.org/for-women/sexual-health-menopause-online/causes-of-sexual-problems/depression-mood-swings-anxiety
- Norton, A. (2022, May 25). Many Older Women Have Active Sex Lives, But Menopause Can Interfere. Consumer Health News | HealthDay. https://consumer.healthday.com/5-18-many-older-women-have-active-sex-lives-but-menopause-can-interfere-2657310459.html
- Stöppler, M. C. (2016, July 19). Healthy Aging: Better Sex After 50. eMedicineHealth. https://www.emedicinehealth.com/slideshow_pictures_senior_health_sexual_problems/article_em.htm
- The North American Menopause Society. (n.d.). How Do I Know I’m in Menopause? https://www.menopause.org/for-women/menopauseflashes/menopause-symptoms-and-treatments/how-do-i-know-when-i’m-in-menopause-
- University of Washington. (2016). Aging with a Disability: Tips for your Sex Life | Rehabilitation Research and Training Center on Aging with Physical Disabilities. Healthy Aging & Physical Disability RRTC. https://agerrtc.washington.edu/index.php?q=info/factsheets/sex
- Williams, M. E., & Fredriksen-Goldsen, K. I. (2014). Same-Sex Partnerships and the Health of Older Adults. Journal of Community Psychology, 42(5), 558–570. https://doi.org/10.1002/jcop.21637